Piles, commonly known as hemorrhoids, can significantly impact your quality of life. For those suffering from this painful condition, surgery is often the most effective treatment.
Dr. Pramod D. Bahekar, a leading Piles Surgeon and Endoscopist with over 35+ years of experience, offers advanced piles surgery treatment in Dombivli. He is also a Senior Consulting general Surgeon, FICS (Fellow of International College of Surgeons), FAIS (Fellow of Association of Surgeons of India, FISCP Fellow of International Society of Coloproctology, FIAGES (Association of GI Endo-Surgeons ), FAMASI (Association of minimal access surgeons of India).
In this guide, we will explore the various aspects of piles surgery, the expertise of Dr. Bahekar, and why his clinic is the best choice for those seeking relief from piles and fistula problems.
What are Piles?
Piles, or hemorrhoids, are swollen veins in the lower part of the rectum and anus, causing discomfort, pain, and sometimes bleeding.
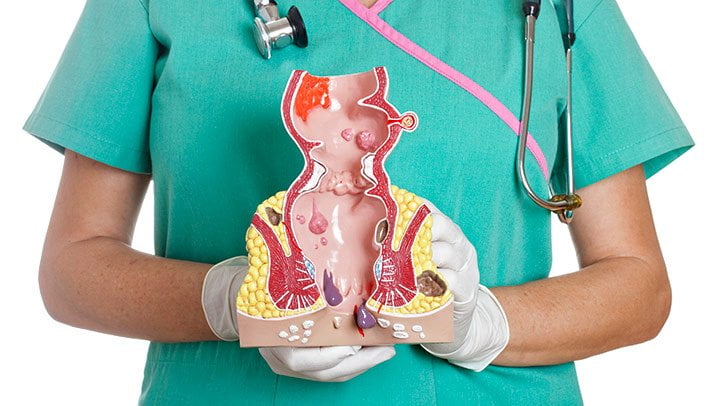
The condition can be classified into two types:
Internal Piles: Located inside the rectum, often painless but can cause bleeding.
External Piles: Found around the anus, leading to pain, swelling, and irritation.
Common Causes of Piles
Several factors contribute to the development of piles, including:
- Chronic constipation or diarrhea
- Prolonged sitting or standing
- Obesity
- Pregnancy
- Straining during bowel movements
Symptoms of Piles:
If you are experiencing any of the following symptoms, it may be time to consult a piles doctor with laser surgery in Dombivli:
- Pain or discomfort during bowel movements.
- Itching or irritation around the anus.
- Bleeding during bowel movements.
- Swelling or lumps near the anus.
- Lump near the anus, which may be sensitive or painful.
Types of Piles Surgery
Piles surgery has evolved over the years, offering patients various treatment options depending on the severity of their condition.
The most common surgical treatments include:
- Laser Surgery
Laser surgery is a minimally invasive procedure that uses laser energy to shrink and remove hemorrhoids. This method is highly effective and offers several benefits, including:
- Minimal pain and discomfort
- Reduced risk of complications
- Faster recovery time
Dr. Pramod D. Bahekar is a leading piles doctor with laser surgery in Dombivli, providing expert care to patients seeking a quick and effective solution.
- Hemorrhoidectomy
Hemorrhoidectomy involves the surgical removal of hemorrhoids. This traditional method is usually reserved for severe cases where other treatments have failed. While effective, it typically requires a longer recovery period compared to laser surgery.
- Stapled Hemorrhoidopexy
This procedure involves using a stapling device to reposition and remove the hemorrhoidal tissue. It is less painful than a hemorrhoidectomy and has a faster recovery time.
When to Consult a Piles Specialist
If the symptoms persist or worsen, it’s crucial to seek help from a piles specialist with laser surgery in Dombivli. Early diagnosis and treatment can prevent complications and make the recovery process smoother.
Benefits of Choosing Laser Surgery for Piles
Opting for piles laser surgery offers several advantages over traditional methods, including:
- Precision: The laser precisely targets the affected tissue, minimizing damage to surrounding areas.
- Less Pain: Patients experience less pain during and after the procedure.
- Quick Recovery: Most patients can return to their normal activities within a few days.
- Outpatient Procedure: Laser surgery is typically performed on an outpatient basis, allowing patients to go home the same day.
Why Choose Dr. Pramod D. Bahekar for Piles Surgery Treatment?
Over 35+ Years of Expertise
With over two decades of experience, Dr. Pramod D. Bahekar is recognized as the best piles doctor with laser surgery in Dombivli. His extensive experience ensures that patients receive the highest standard of care, tailored to their specific needs.
Top Facilities at Amrut Hospital
Amrut Hospital, where Dr. Bahekar practices, is equipped with the latest medical technologies. The hospital offers a dedicated piles clinic with laser treatment in Kalyan and Dombivli, providing patients with access to cutting-edge treatments in a comfortable and modern setting.
Personalized Patient Care
Dr. Bahekar is committed to providing personalized care to each patient. From the initial consultation to post-operative care, he ensures that every aspect of the treatment process is handled with the utmost professionalism and compassion.
Positive Patient Outcomes
Dr. Bahekar’s expertise in piles surgery has led to numerous positive outcomes for his patients. Many have praised his ability to relieve their symptoms and improve their quality of life, making him a trusted piles specialist with laser surgery in Dombivli.
Post-Operative Care and Recovery
After the surgery, Dr. Bahekar will provide detailed post-operative care instructions. These may include:
- Pain Management: Medication to manage any discomfort.
- Dietary Guidelines: Recommendations on foods to eat and avoid.
- Activity Restrictions: Guidance on when to resume normal activities.
- Follow-Up Visits: Scheduled appointments to monitor your recovery.
Conclusion
Piles surgery treatment, particularly laser surgery, offers a safe and effective solution for those suffering from hemorrhoids. With over 22 years of experience, Dr. Pramod D. Bahekar is the piles doctor with laser treatment in Dombivli East that patients trust for expert care.
His commitment to patient well-being, combined with top facilities at Amrut Hospital, ensures that you receive the best possible treatment for your condition.
Schedule a consultation
If you’re seeking relief from piles, don’t hesitate to schedule a consultation with Dr. Pramod Bahekar, the best piles doctor with laser surgery in Dombivli.
Take the first step towards a pain-free life by contacting Amrut Hospital today.